01.10.2021 - Inequalities in Cancer Care in CEE

Friday, October 1st
14:00-15:30 CEST
Venue: GLOBSEC OFFICE (Approx. 30 participants) & Zoom platform - Please register here in advance to join the webinar on Zoom.
The event will be live-streamed on our social media channels and on the video tile below
Panel discussants:
- Antonella Cardone (European Cancer Patients Coalition, Brussels – Director)
- Hana Horka (Europe’s beating cancer plan Taskforce, DG SANTE, Brussels – Policy Officer)
- Univ. Professor Dr Dr.h.c. Christoph Zielinski (Vienna Cancer Center & Central European Cooperative Oncology Group (CECOG) - President)
- Martin Smatana (GLOBSEC Health Fellow, Health Data Analyst, Institute of Health Data Policies at MoH of Slovakia-former director)
- Štefan Korec, M.D. (Clinical Oncologist, Medical Expert with experience from EU & US, Patients organization OnkoAliance Slovakia – Executive Director)
Moderator: John Barter, Senior Vice President of GLOBSEC
Other active discussants from the wider CEE region are expected. EC representatives, EP members, Parliamentary Members, Ministry of Health & National Public Health representatives, Medical Experts, Patients Organizations, Professional Associations, Health Insurance Companies, Private Sector representatives targeted audience.
Topical angles for webinar discussion:
- Importance of accurate – up to date information on cancer treatment across CEE
- Variability of screenings – usage of different methods and testings
- Unequal access to certain cancer treatments in between CEE countries (surgery, radiology, medicines) e.g. only 1/3 (31) out of 95 innovative oncology drugs approved by EMA in the period 2011-2020 are currently available to patients in Slovakia
- Shortages of medicines & access to innovative treatments, HTA, delays to approvals
- Fragmented palliative care across the society and countries difference, cancer survivorship and rehabilitation
- Very poor governance, preparedness in oncology health planning, cancer control within each CEE country
- Underresourced systems, cost of cancer treatment, under-resourced personal resources
Data confirms that Cancer is a significant cause of morbidity and mortality in high, middle and low-income nations across the world. In the majority of the EU countries, Cancer has now overtaken cardiovascular disease as the leading cause of premature death.
The number of new cancer cases and increasing death rates across all EU 27 countries are not the sole alarming figures we perceive. Even more revealing are the evident disparities between different European nations.
The most recent analysis of cancer survival data across Europe provides irrefutable evidence that cancer survival rates vary significantly between different European countries (Picture 1.).
Picture 1.:
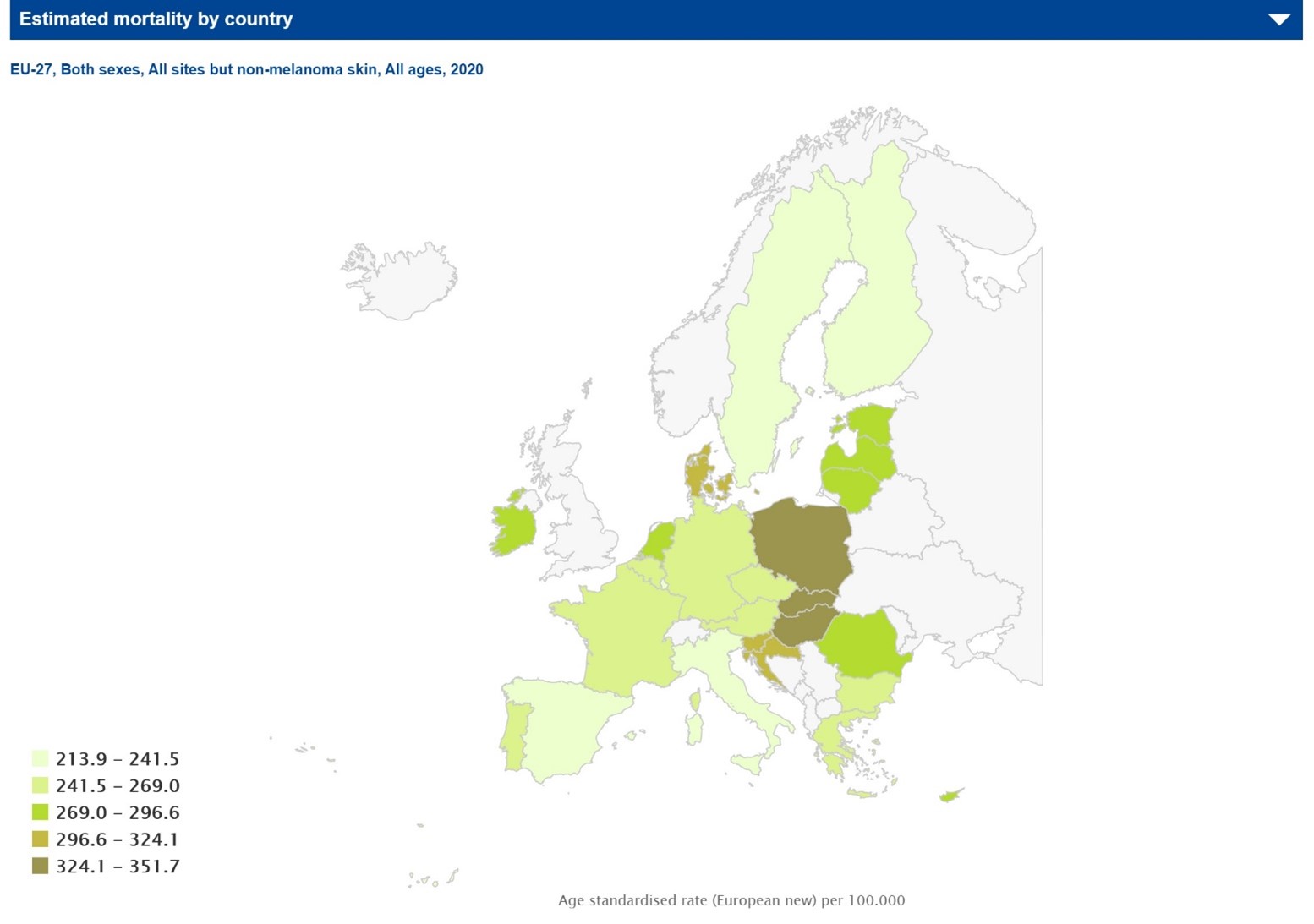
Thus there are significant differences in changes in survival following treatment of different types of cancers in between patients across the EU, from North to the East, West to the east East or South. Whether it be preventable (e.g. cervical cancer), curable (e.g. certain forms of breast cancer, childhood leukaemia), or poor prognosis (e.g. ovarian, pancreatic cancer), European inter-country variations in cancer survival rates are significant and also regional intra-country variations are also evident, leading to differences in survival within individual countries.
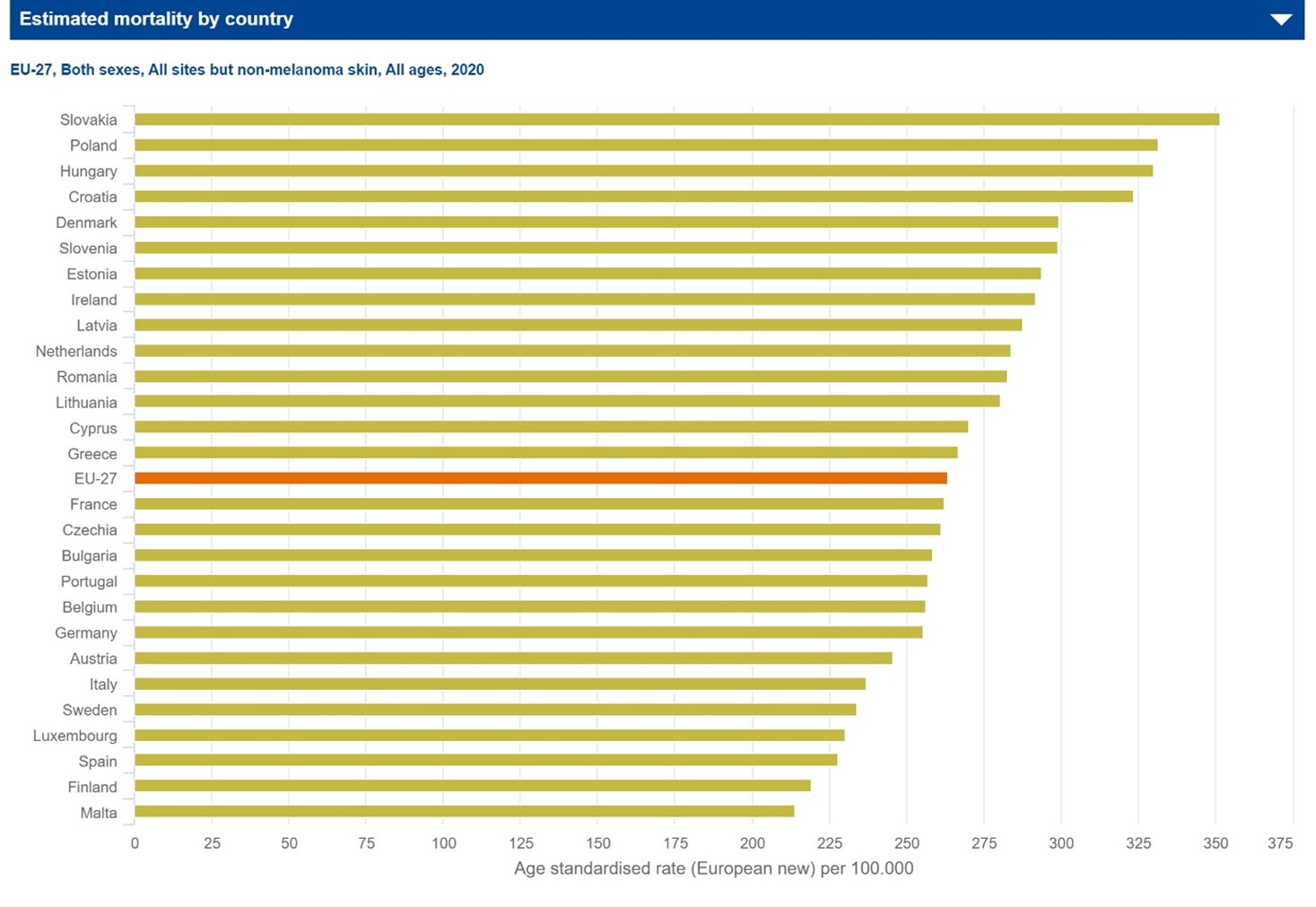
The situation in Eastern Europe is particularly challenging, with mortality rates for many cancers above the European average (Picture 2).
Picture 2.:
The role of cancer inequalities in the Europe of disparities
Inequalities are at the heart of many of these profound disparities that are experienced by European citizens. Key patient needs that must be addressed across Europe include:
- a deficiency in accurate, up-to-date information that is patient-accessible
- extreme variability in cancer screening services
- unequal access to curative cancer treatments (surgery, radiation, medicines)
- fragmented cancer rehabilitation services
- poor governance, major organisational, structural and fiscal deficits in health planning
- the lack of a citizen-focused European cancer survivorship plan
Additionally, in many EU 27 Member States, National Cancer Control Plans are lacking or are inadequately resourced, underpinning both inter-and intra- country disparities in survival, quality of care and patient rehabilitation.
Social and economic deprivation and the influence of recent austerity measures and the impact of COVID-19 pandemics restrictions further exacerbate many of these inequalities. For cancer patients to get the treatment that they both require and deserve, a multidisciplinary team-based strategy must be adopted for all member states, providing a patient-centred approach that addresses all aspects of the cancer journey, with increasing emphasis on survivorship issues including psychosocial support and improved Quality of Life, delivered within a framework where patients’ rights and views are respected and acted upon.
An important consideration for developing and implementing approaches that address the inequalities underpinning the Europe of Disparities in Cancer is the need for accurate and comprehensive cancer incidence/survival data. Capturing this data at an entire population level is critical. Data coverage across Europe is suboptimal, varying from 17 to 100% (average 50%) and must be improved and harmonised to inform future cancer policy.
According to recent data by European Cancer Organisation (ECO), the following recommendations for making a change into the reality of “ Intelligence as an Enabler“ in the Central and Eastern Europe environment could be applied:
Recommendations & objectives:
- IMPROVE CANCER INTELLIGENCE - inform an evidence-based approach to decision making and policy for affordable, high-quality and equitable cancer control
- INVEST IN RESEARCH, EDUCATION AND TRAINING - develop expertise and retain cancer professionals in the clinical, nursing and allied communities
- DEVELOP AND STANDARDISE PATIENT PATHWAYS - enhance the quality of care across the continuum from diagnosis through to treatment and end-of-life care, while optimising the use of resources
- ENHANCE CAPACITY BUILDING FOR PATIENT ORGANISATIONS - play a role in promoting healthy behaviours, targeting risk factors such as smoking, obesity and alcohol consumption, as well as increasing public awareness of cancer care financing and organisation
The key enablers for Central and Eastern Europe:
- Robust Cancer intelligence
- Resilient National Cancer Control Plans (NCCPs)
- Patient-centred multidisciplinary teams
- Research and innovations empowered culture
ECO recommended implementing the “Cancer Country Dashboards“ – Intelligence tool to help Policy Change. Cancer country dashboards could capture key intelligence, underpinning cancer policy decision-making and monitoring progress, locally, nationally and regionally. Another tool would be to develop cancer “learning environment” which would benefit the entire CEE region.
Source of data: